
How TMS Helps Military Members & Dependents?
How TMS Helps Military Members & Dependents?
Mental health challenges affect many military families, often impacting both the service member and their loved ones. The pressures of military life, exposure to trauma, frequent relocations, and long separations can cause emotional distress that doesn’t always respond well to traditional treatment methods. Transcranial Magnetic Stimulation (TMS) is now emerging as a life-changing therapy, offering hope and healing without the need for medication or invasive procedures.
This article explores how TMS therapy is transforming mental health care for military personnel and their dependents, the process involved, its unique advantages, and how clinics like Karma Doctors & Associates are making TMS Therapy in Palm Springs accessible for military families.
Understanding the Emotional Strain of Military Life
Military service demands physical endurance and mental resilience, but constant exposure to stress and danger can lead to emotional exhaustion. Even when a service member returns home, the emotional impact often lingers.
Some common challenges faced by military families include:
- Difficulty adjusting after deployment
- Strained relationships due to long separations
- Emotional numbness or withdrawal
- Sleep problems affecting daily life
- Chronic stress impacts both the service member and their loved ones
Dependents, including spouses and children, may also face anxiety, depression, or feelings of instability due to frequent relocations and the fear of losing a loved one in service. These struggles highlight the need for effective mental health solutions beyond traditional therapy and medication.
Understanding TMS
Transcranial Magnetic Stimulation (TMS) is a non-invasive treatment that uses magnetic pulses to activate specific brain regions linked to mood control. Unlike medications that affect the whole body, TMS focuses directly on the brain areas that regulate emotions, making it a targeted and highly effective option for various mental health issues.
TMS is FDA-approved for depression and has shown positive results for conditions like post-traumatic stress disorder (PTSD), Anxiety, and sleep disturbances—all of which are commonly reported in military communities.
Why TMS is Especially Beneficial for Military Families
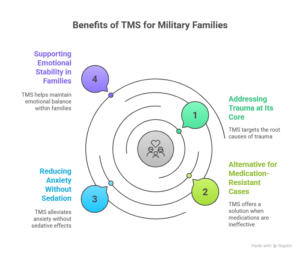
Military members and their dependents often face unique emotional challenges that make TMS particularly helpful:
1. Addressing Trauma at Its Core
Traumatic experiences from combat or high-stress missions can leave a deep imprint on the brain. TMS helps reawaken underactive brain regions affected by trauma, allowing individuals to process emotions more effectively and reduce flashbacks or intrusive thoughts.
2. An Alternative for Medication-Resistant Cases
Many service members and family members try antidepressants but experience limited relief or severe side effects. TMS offers a drug-free solution, minimizing the risk of dependency or unwanted reactions.
3. Reducing Anxiety Without Sedation
For dependents struggling with anxiety caused by constant relocations or fear for their loved one’s safety, TMS calms overactive brain circuits without the sedative effects that medications often cause.
4. Supporting Emotional Stability in Families
When one family member struggles mentally, it affects the entire household. TMS can help military members and dependents improve mood and emotional balance, strengthening family bonds.
How a Typical TMS Treatment Works
TMS therapy involves a series of sessions conducted in a clinical setting. The procedure is simple, painless, and requires no downtime. Here’s what to expect:
- Step 1 – Initial Assessment: A mental health professional evaluates your symptoms and history to confirm eligibility for TMS.
- Step 2 – Treatment Planning: The provider identifies the exact brain area to target and sets up the treatment schedule.
- Step 3 – Daily Sessions: A small device is placed on the scalp, delivering gentle magnetic pulses. Each session lasts 20–40 minutes and is repeated over several weeks.
- Step 4 – Progress Tracking: Improvements are monitored, and adjustments are made if needed to maximize results.
Patients can return to their daily routine immediately after each session, making it a convenient option for busy military families.
Transformative Effects of TMS on Mental Well-being
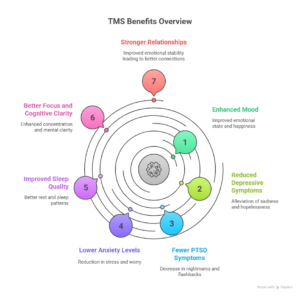
Military members and their families often report noticeable improvements after completing a TMS program:
- Enhanced mood and reduced depressive symptoms
- Fewer PTSD-related nightmares and flashbacks
- Lower anxiety levels
- Improved sleep quality
- Better focus and cognitive clarity
- Stronger relationships due to emotional stability
These benefits not only help individuals recover but also foster a healthier home environment for their dependents.
The Future of Mental Health Care for Military Families
TMS represents a new chapter in treating mental health conditions linked to military life. As research continues to highlight its effectiveness, more veterans, active-duty members, and dependents are turning to TMS to reclaim their mental well-being. With its non-invasive approach and proven results, TMS is becoming a trusted alternative for those who have not found success with traditional therapies.
Frequently Asked Questions
1. Can military dependents also access TMS therapy?
Yes, TMS is not limited to service members. Dependents experiencing depression, anxiety, or stress-related issues can also benefit from treatment.
2. Does TMS therapy hurt?
No, TMS is a painless procedure. Some people feel a tapping sensation on the scalp, but it’s well-tolerated and does not require anesthesia.
3. How soon can results be seen?
Improvements are often noticeable within 2–4 weeks, though full benefits usually appear after completing the treatment course.
4. Is TMS safe for someone already on medications?
Yes, TMS can be used alongside medications and therapy, or as a standalone treatment for those who prefer a drug-free option.
5. How long do the effects of TMS last?
Many patients experience long-lasting relief. Some may need occasional maintenance sessions, depending on the severity of their condition.



